What is Interprofessional Practice?
You’re busy! With heavy workloads and demanding schedules, audiologists and speech-language pathologists (SLPs) already face enough challenges in their daily practice. You don’t need one more thing to worry about. Interprofessional practice (IPP) can seem like just more meetings and additional paperwork. However, this collaborative approach can actually help you work more efficiently with colleagues and improve the care you give patients and students. Learn more about what IPP means for you.
What is IPP?
As audiologists and SLPs, we always strive to improve outcomes for the people we serve. In today’s world of specialized care, this requires collaboration with professionals in other disciplines—as well as with families and caregivers. Interprofessional practice (IPP) is a framework that makes this collaboration more successful.
How is IPP collaboration different?
Audiologists and SLPs regularly collaborate with other educational and medical professionals. But IPP isn’t just having more meetings or sending more emails. It’s an intentional approach to collaboration. The IPP framework helps professionals learn about, from, and with colleagues from different specialties.
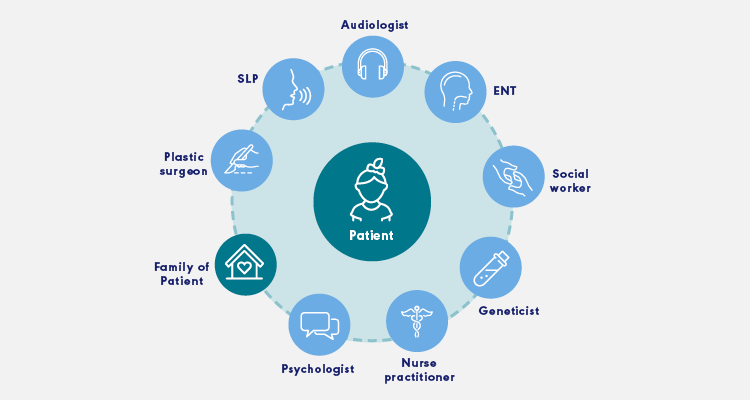
On successful IPP teams, each member provides their professional expertise and works together on an assessment and treatment plan that centers around the person and their family. Teams collaborate on planning and developing solutions, taking into account each member’s perspective.
Participating in an IPP team can take many forms. In some cases, the collaboration is short term; other times, it requires ongoing support over several years. In some instances, more professionals are added to the IPP team for a specific need or when existing team members want additional expertise. For example, in this case study, a school IPP team brought in an SLP from a local university to help evaluate a student with cerebral palsy; the SLP had expertise in augmentative and alternative communication (AAC). For examples of IPP teams in action, see the case studies.
This video features an IPP team from the Kennedy Krieger Institute (Fairmount Campus) in Baltimore, Maryland, describing how they work together on an IPP team. They explain how working collaboratively benefits their students.
![]()
What skills do I need for IPP?
The most important aspect of IPP is collaboration. IPP is not a one-off meeting or an email sent out to the team. Rather, true IPP is a collaborative partnership and is built through understanding other members’ disciplines and the value they contribute. Team members support and reinforce each other, helping to ensure that patients, students, and their families understand the importance of each aspect of their treatment and follow through on all recommendations.
Learn more about interprofessional education (IPE), which helps students and working professionals develop the skills they need to work on IPP teams.
The Interprofessional Education Collaborative (IPEC) has outlined the following four main competencies for IPP [PDF]:
Maintaining a climate of mutual respect while working with individuals of other professions.
Using knowledge of one’s own role and that of other professions to assess and address the needs of patients.
Communicating in a responsive and responsible manner that supports a team approach.
Applying relationship-building values and the principles of team dynamics to perform effectively in various team roles to plan, deliver, and evaluate the people they serve with policies that are safe, timely, efficient, effective, and equitable.
To implement IPP in your workplace, see our how-to section.
What’s keeping all audiologists and SLPs from practicing IPP?
Like any new change or initiative, IPP has barriers to adoption. According to the results of ASHA’s 2019 Interprofessional Practice Survey, audiologists and SLPs think that limited time and heavy workloads are barriers to the widespread adoption of IPP. Organizational culture can also be a barrier to successful IPP teams.

According to survey results, lack of time is the top barrier to IPP that audiologists and SLPs encounter. It’s true that IPP does require team meetings and ongoing communication. However, operating in silos results in gaps in patient care—including diagnostic errors, redundancy in services across disciplines, and inaccurate billing. Improving communication may actually reduce work. Learn more about the benefits of IPP.
An organizational culture that doesn’t support IPP can also make adopting the framework a struggle. IPP stresses equality among the team members. This may go against the status quo at some schools or clinics. For example, on an IPP team in a health care setting, the input of an audiologist is just as vital as that of a surgeon. Both perspectives are equally important when it comes to producing the best outcome for a patient.
Why is IPP important in all settings?
Whether you practice in a school, hospital, or private clinic, IPP is an important way to improve outcomes for the people you serve.
Audiologists and SLPs typically work in settings where collaboration is expected. IPP is an intentional approach that involves cooperating with colleagues in other disciplines. One IPP team may include medical professionals working to treat a patient with a rare condition. Another IPP team may involve a group of educators developing and implementing an individualized education program (IEP) for a student with special needs. Ultimately, the goal of IPP is improving outcomes for the people we serve—regardless of where they receive services.














